What if we had a systematic approach to bringing research findings to on-the-ground settings around the world? What if we could ensure that research findings did more than just populate academic journals, and in fact, improved health for millions of people?
Professor Bryan Weiner, PhD, who recently joined the UW Department of Global Health (DGH) to help expand the Implementation Science (IS) program, is trying to do just that. Most recently at the University of North Carolina at Chapel Hill (UNC), Dr. Weiner investigates how we get “what works” to those who need it most. IS focuses on closing the “know-do gap”: the distance between what is known to be effective based on evidence, systematic research, and evaluation methods, and what is done in practice.
That sounds great, but, what does this approach look like in reality? We asked Dr. Weiner to tell us more about the science of implementation, what drew him to Seattle, and his vision for the UW IS program.
Fun fact: I share my birthday (July 26) with Helen Mirren, Carl Jung, Aldous Huxley, the launches of NASA’s Apollo 15 and Discovery, and Liberian Independence Day.
How did you get started in implementation science research?
My training is in organizational psychology, which focuses on people’s behavior in the workplace. Over the past 20 years, I’ve studied the implementation of a wide range of innovative and evidence-based practices in health care organizations, mostly in the US and mostly in non-communicable disease, to understand why implementation succeeds or fails.

I have also introduced new theories and measures for use in IS. One theory responds to a growing concern that many implementation efforts are unsuccessful because leaders fail to establish sufficient “readiness for change” – in other words, whether members of an organization share a resolve to implement a change, and whether they believe they are collectively capable of doing so.
I’m currently working on a project to test this theory by looking at whether establishing “readiness for change” can predict implementation success in primary care practices in the US.
What drew you to UW?
I came here as a strategic hire in IS for the School of Public Health, after leading the IS program at UNC. While other universities have strong domestic or strong international IS programs, very few have both, so the opportunity to work with this community of researchers was most appealing. Moving here allowed me to expand my US-based work to a global context and to actively foster collaboration between the two sub-disciplines—I feel strongly that domestic IS and global IS can and should reciprocally inform each other.
For example, I’m working with Judd Walson and Arianna Means on the DeWorm3 project in India, Benin and Malawi to assess “system readiness” for implementing community-wide mass drug administration (MDA) to halt the transmission of intestinal worms. This is a shift in both setting and scale from the typical school-based MDA programs for children, to treating entire communities. We’re adapting measures that I developed in the US context to assess the readiness of stakeholder groups and organizations at various levels—from the ministries of health and education, to the local village leaders—to implement this alternative approach. We want to understand whether “readiness” in other countries means the same thing as it does in the US, how cultural context impacts how we measure it, and whether it can still predict implementation success in different countries.

As I said, learnings can and should go both ways—we’ve seen strong evidence supporting the role of community health workers globally to provide basic health and medical care outside of a clinic or doctor’s office. We don’t tend to employ such a model in the US, even though community health workers could help address issues like chronic care needs between doctor visits.
IS is a relatively new field, so it’s exciting to think about the ways domestic-global cross-fertilization can help strengthen it.
How do you know when you’re succeeding?
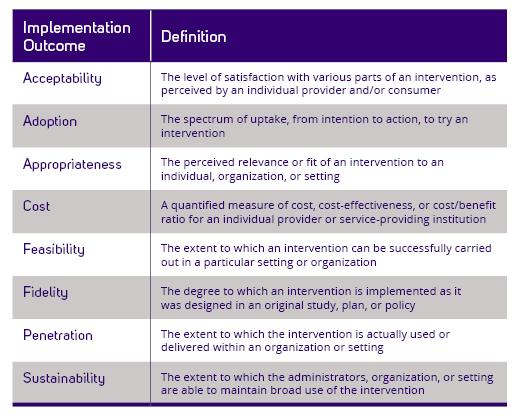
In health care IS, we’re looking for improved health through consistent, high-quality and evidence-based program delivery. A health intervention may work in a small-scale trial, but often there are challenges with expanding the intervention to other settings that make it less effective. If a program or approach is successful in a research setting, it doesn’t necessarily translate into a real world setting. Additionally, an intervention may work well in a clinical setting in one country but may not work well once implemented in another country with different social or structural considerations. Ultimately, we measure success by “implementation outcomes”, or the results of deliberate efforts to implement new treatments, practices, or services (see diagram).
The sweet spot for IS is taking “what works,” figuring out how much it can be adapted without losing its effectiveness, and then scaling it up to reach large numbers of people who could benefit from it.
Is there a project you’re particularly excited about?
Carey Farquhar is working in Western and Central Kenya on the Assisted Partner Notification Study (APS), which attempts to contact the sexual partners of consenting patients living with HIV and asks them to come to the clinic for testing. Over 50% of people living with HIV in Kenya are unaware of their status, yet under national guidelines a partner might merely receive a letter in the mail asking them to come in. APS employs a more active strategy by immediately contacting sexual partners to notify them of exposure, offer HIV testing, and link to care if the results are positive.
Implementation science helps optimize this approach by identifying key elements needed for the notification service to be effective in other locations, as well as its associated cost. This information can be used by policy makers, clinic managers, and public health practitioners to determine whether the implementation will succeed in their particular setting.
What have you been up to since joining the DGH?
I’ve been really enjoying getting to know everyone. I have worked on 13 grant applications with colleagues in DGH and Health Services since August! Coming up with research ideas, thinking through study designs, and writing research proposals are great ways to learn how my colleagues approach problems, and there is always a new perspective. While not all will, some of these grants will get funded, so I look forward to the next phase of these collaborations!

What do you do for fun?
I enjoy doing yoga, walking my dogs, and cooking. Since my wife and I moved here last summer, we have tried to get out and explore Seattle every weekend. Now that we have settled in West Seattle, we look forward to venturing beyond the city and exploring the Pacific Northwest. Our daughter is at UCLA, experiencing her very first year of college. We are excited to be on the West Coast where we can get down to California every so often to visit her and other family members.

(By Alex Murphy)